Procedure
-
Cosmetic Procedures

A focus on cosmetic procedures is used in all applications in the clinic.
-
Diathermy & Curettage
Diathermy and Curettage is a treatment using a semi sharp instrument to scrape out the cancerous tumour and uses diathermy to destroy a further margin of surrounding tissue and stop bleeding.
-
Ellipse Excision
Ellipse excision is the simplest and commonest form of surgical treatment and involves cutting out a boat shaped section of skin containing the cancer, and then using sutures to bring the edges together.
-
Flap Surgery
Flap surgery is a plastic surgical technique which is used for treatment of skin cancers where a simple ellipse would not suffice.
-
How do I reduce scaring from my recent skin cancer removal?
The Melanoma Scan doctor and nurse will give you detailed instructions on how to care for your wound to reduce scarring.
Any procedure to remove a skin cancer will cause a scar and some people will scar more than others depending on their tendency towards keloid scarring and their skin type. Scars tend to settle to a pale mark, either an oval area after curettage and cautery or as a line from excisional skin surgery. If there is a lot of background sun damage, this pale area can become more prominent and noticeable. Background sun damage can include solar keratosis, freckles, pigmentation, age spots and telangiectasias (dilated small vessels on the skin surface). All of these lesions can be treated, either as individual lesions or as part of a field treatment such as edit, PDT, lazer, IPL or skin peels.
-
How long do I need to keep my wound covered after surgery?
There are a variety of wound care regimes used after surgery. Some areas are difficult to cover, and may be left without a dressing and the wound covered with antibiotic ointment. This may include scalps, eyelids and beard areas. Most wounds benefit from being covered because it can keep the area clean and help wick away any blood or fluid leaking from the wound. Our routine wound dressing involves application of antibiotic ointment, kaltostat (a dressing that reduces bleeding), then a protective dressing. This can be left intact until removal of suture time in 7 days if kept clean and dry. An ice pack or pressure dressing may be applied if necessary to reduce bleeding risk and protect the area.
Skin Cancer Aftercare Guide: Tips for Non-Melanoma Skin Cancer
Skin cancer is a serious condition that affects millions of people worldwide. Understanding the various aspects of skin cancer, including non-melanoma skin cancer, is crucial for effective treatment and aftercare. Non-melanoma skin cancer develops when abnormal skin cells grow uncontrollably. These cancer cells can form tumours and invade surrounding tissues if not treated promptly. The most common types of non-melanoma skin cancer are basal cell carcinoma and squamous cell carcinoma.
After undergoing skin cancer treatment, proper post-treatment care is essential for effective healing. Wound care post-excision or curettage involves keeping the wound clean and moist to promote healing. It is important to wash the wound gently with mild soap and water, pat it dry and apply antibiotic ointment or petroleum jelly to prevent infections. Covering the wound with a bandage helps protect it from external elements and speeds up the healing process.
During the healing process, it is crucial to monitor the signs of proper healing after skin cancer treatment. These signs include the formation of a scab, which indicates that the wound is healing. It typically takes several weeks for scars to heal post-skin cancer removal. To aid in the healing process, it is essential to follow the dermatologist's instructions carefully, avoid exposing the wound to sunlight and refrain from picking at the scab.
To prevent complications during the skin cancer aftercare period, it is important to take steps to avoid infections around the wound site. Following recommended wound care practices and keeping the wound clean and covered can help reduce the risk of infections. If any signs of infection, such as redness, swelling or pus, develop, it is crucial to seek medical attention promptly to prevent further complications.
Long-term skin cancer management involves regular follow-up appointments with a dermatologist to monitor any changes in the skin and detect potential issues early. Skin cancer survivors should also take proactive measures to protect their skin from future skin cancer development. This includes wearing sunscreen, avoiding excessive sun exposure and regularly examining the skin for any changes or abnormalities.
For basal cell and squamous cell skin cancers, specific aftercare strategies are recommended to promote healing and reduce the risk of recurrence. These may include using antibiotic ointments, keeping the wound moist and following proper wound care practices. It is essential to call your doctor if you experience any unusual symptoms or complications during the healing process to ensure that the cancer has been completely removed and to address any issues promptly.
Q: What is the purpose of a skin cancer aftercare guide?
A: The purpose of a skin cancer aftercare guide is to provide tips and instructions for wound care after procedures such as excision, cryotherapy or photodynamic therapy.
Q: What is the importance of wound care in skin cancer aftercare?
A: Proper wound care is crucial in skin cancer aftercare to prevent infections, promote healing and minimise scarring.
Q: How can stitches affect wound healing after skin cancer surgery?
A: Stitches are commonly used to close the incision after skin cancer surgery, and their proper care is essential for ensuring the wound heals correctly.
Q: What are some tips for caring for wounds following skin cancer removal?
A: Tips for wound care after skin cancer removal include keeping the area clean, changing dressings regularly, avoiding strenuous activities and following your healthcare provider's instructions.
Q: How long does it typically take for a wound to heal after skin cancer surgery?
A: The time it takes for a wound to heal after skin cancer surgery varies depending on the type and location of the surgery, but it usually takes a few weeks to a few months.
Q: Are there any signs of complications that should be reported to a healthcare provider after skin cancer surgery?
A: Signs of complications such as infection, slow healing, excessive bleeding or increasing pain should be reported to your healthcare provider immediately.
Q: Can cryotherapy be used as a treatment for skin cancer?
A: Cryotherapy, which involves freezing the cancerous cells, can be used as a treatment for certain types of skin cancer, especially for superficial skin cancers.
Q: What is photodynamic therapy and how is it used in the treatment of skin cancer?
A: Photodynamic therapy is a treatment that involves applying a photosensitising agent to the skin and then exposing it to a light source to activate the agent and destroy cancer cells. It is used in the treatment of certain types of skin cancer.
For further information, please feel free to Contact Us or follow the link to request an appointment by clicking Book Now.
-
How long does it take to have a cosmetic mole removal?
Mole removal occurs in two ways, either a shave excision, which is very quick, or a formal ellipse excision, which takes a little longer. Shave excision is a technique that involves putting a small amount of local anaesthetic under the mole and then using either a straight or curved blade, which is passed through the skin directly under the mole, resulting in the mole being removed with a narrow margin of normal tissue under and around it. Occasionally, if the mole is being removed for benign reasons (for example, it is raised and gets in the way of shaving and repeatedly traumatised) the doctor may remove the raised part of the mole and leave a small amount of mole tissue behind, in an effort to minimise any visible scar or depression left by the mole removal. This procedure normally takes between two minutes and 5 minutes to do, using a low-sting local anaesthetic, which has the dual advantages of hurting less and giving almost immediate numbing to superficial lesions like a mole. This type of mole removal can often be incorporated into a skin check or 15-minute procedure time.
Formal ellipse excision takes a little longer, because a larger area of skin needs to be numbed, and a formal excision setup needs to be done by the doctor or nurse. The mole needs to be removed as an ellipse of skin (a boat-shaped piece of skin removed) and the wound sutured, usually in two layers, closing both deep and superficial parts of the skin, minimising the risk of scar stretching and tram track marks being left behind from the sutures. A typical mole removal using this technique takes about fifteen minutes to perform when assisted by a nurse, or 25 minutes without the assistance of a nurse.
Having a mole is a common occurrence for many individuals, as these small coloured spots on the skin are usually harmless. However, in some cases, mole removal may be necessary for both health and cosmetic reasons.
What is a Mole and Why Does It Need Removal?
Understanding the Nature of Moles on the Skin
A mole, also known as a nevus, is a growth on the skin that can appear anywhere on the body. Most moles are harmless and are usually brown or black in colour. They are made up of cells called melanocytes, which give the mole its pigmentation.
When Should You Consider Removing a Mole?
While most moles are benign, some may need to be removed if they show signs of change in size, shape, or colour. If a mole becomes itchy, and painful, starts bleeding, or exhibits asymmetrical borders, it is important to have it checked by a dermatologist.
Possible Risks Associated with Untreated Moles
Untreated moles that exhibit abnormal characteristics could potentially develop into skin cancer, particularly melanoma. Timely removal of suspicious moles can help prevent the progression of skin cancer.
Process of Mole Removal and Treatment Options
Types of Mole Removal Procedures Available
There are different methods of removing moles, including excision, laser therapy, shave excision, and radiofrequency ablation. The chosen method depends on the size, shape, and location of the mole.
Comparison of Cosmetic Mole Removal Techniques
Cosmetic mole removal techniques aim to remove the mole with minimal scarring. Laser mole removal and shave excision are popular cosmetic procedures that offer precise removal of moles with reduced scarring.
Discussing Treatment Options with a Skin Doctor
It is essential to consult a dermatologist to discuss the best treatment option for mole removal based on the individual's skin type, the mole's characteristics, and the desired outcomes.
Healing Process and Scar Care After Mole Removal
Expected Healing Time After Mole Removal
The healing time after mole removal varies depending on the method used and the size of the mole. Generally, it takes a few weeks for the skin to heal completely.
Scar Formation and Scar Healing Remedies
After mole removal, a scab will form, which will eventually fall off, leaving behind a scar. To aid in scar healing, applying silicone-based gels, keeping the scar moisturized, and protecting it from the sun can help minimize scarring.
Tips for Minimizing Scarring After Mole Removal
To reduce scarring after mole removal, it is important to follow post-procedure care instructions provided by the dermatologist, avoid picking at the scab, and keep the area clean and protected from infection.
Skin Cancer Concerns and Moles: What You Need to Know
Link Between Skin Cancer and Moles
Skin cancer, particularly melanoma, can develop from abnormal moles. Regular skin checks and monitoring moles for any changes are crucial in the early detection and treatment of skin cancer.
Identifying Signs of Melanoma in Moles
Signs of melanoma in moles include asymmetry, irregular borders, uneven colour distribution, and changes in size. If a mole shows any of these signs, immediate medical attention is necessary.
Importance of Timely Treatment for Suspicious Moles
If a mole appears suspicious or displays concerning features, such as rapid growth or changes in appearance, it is essential to seek professional evaluation and prompt treatment to prevent potential skin cancer development.
Scheduling Your Mole Removal Appointment and Aftercare
How to Book an Appointment for Mole Removal
To schedule a mole removal appointment, individuals can contact a skin specialist or a skin cancer clinic to arrange a consultation and discuss the removal procedure.
Preparation Steps Before Mole Removal Procedure
Prior to the mole removal procedure, patients may need to follow specific pre-operative instructions, which may include avoiding certain medications and preparing the skin surrounding the mole.
Post-Procedure Care for Optimal Healing and Recovery
After mole removal, following post-procedure care instructions, such as keeping the area clean, applying recommended ointments, and attending follow-up appointments, is essential for optimal healing and scar care.
Q: What is skin mole removal?
A: Skin mole removal is a procedure to remove moles from the skin that may be concerning or unwanted. It can be done for both cosmetic reasons and to prevent skin cancer.
Q: What is the healing time after mole removal?
A: The healing time after mole removal can vary depending on the method used and the size of the mole. It usually takes a few weeks for the skin to completely heal.
Q: What are the risks of scarring after mole removal?
A: Scarring after mole removal is a common concern, especially if the mole is large or located in a prominent area. However, with proper care and follow-up, scarring can be minimized.
Q: Is cosmetic mole removal an option?
A: Yes, cosmetic mole removal is an option for those who wish to have moles removed for aesthetic reasons. It can help improve the appearance of the skin and boost self-confidence.
Q: How can I book an appointment for mole removal?
A: You can book an appointment for mole removal by contacting a skin doctor or specialist skin clinic that offers mole removal services. They will assess your mole and recommend the best course of action.
Q: What is the process for scar healing after mole removal?
A: Healing after mole removal involves keeping the area clean and protected, following any post-procedure care instructions provided by your doctor, and monitoring the site for any signs of infection or complications.
Q: What are the different methods of mole removal?
A: The different methods of mole removal include surgical excision, laser removal, and cryotherapy. The method used will depend on the size and location of the mole, as well as other factors.
IS IT A STANDARD PROCEDURE TIME?
A shave excision can be done in a standard 15-minute appointment, however, an ellipse excision is usually booked into a 30-minute procedure appointment, so it depends on the technique that you have discussed with your doctor.
MELANOMA SCAN - SKIN CANCER CLINIC
For further information, please feel free to Contact Us or follow the link to request an appointment by Book Now.
-
I have been diagnosed with skin cancer, what’s next?
After a diagnosis of skin cancer the doctor will discuss treatment options, which may be as simple as a 5 minute procedure to perform curettage and cautery to the lesion, or a surgical procedure to formally excise the lesion with appropriate margins. Most excisions are done as an elipse and suture ie the lesion is cut out as a boat shape of skin, and the edges brought together using a combination of deep dissolving and superficial sutures which are removed a week later. Occasionally for more difficult or cosmetically sensitive areas, a flap or a graft may need to be used to maintain a normal appearance or function post skin cancer excision. Sometimes radiotherapy or further testing may be needed for high risk lesions.
What is Radiotherapy?
Radiotherapy is often used where there is an inoperable lesion or where surgery is not practical such as peri- neural invasion of cancer. High risk cases of melanoma may warrant testing with CT scans, PET scans, or sentinel lymph node biopsy.
Your doctor will inform you about the nature of the cancer you have and if further testing and or treatment is necessary.
Skin Cancer and Melanoma Skin Cancer Diagnosis
What are the symptoms of skin cancer?
Skin cancer can manifest in various ways, but common signs include changes in the size, shape or colour of moles or spots on the skin. It is essential to be vigilant for any new growths, sores that do not heal, or unusual bleeding, as these could be indications of skin cancer.
What are the different types of skin cancer?
Skin cancer is broadly categorised into melanoma and non-melanoma skin cancer. Melanoma is a serious type of skin cancer originating from melanocytes, while non-melanoma skin cancers, such as basal cell carcinoma and squamous cell carcinoma, are more common but generally less aggressive.
How is skin cancer diagnosed?
Diagnosis of skin cancer typically involves a skin examination by a healthcare provider, where suspicious areas are assessed. If necessary, a skin biopsy may be recommended to confirm the presence of cancer cells and determine the type of skin cancer.
What are the treatment options for skin cancer?
Treatment options for skin cancer depend on various factors, such as the type and stage of cancer. Common approaches include surgery to remove cancerous tissue, radiation therapy to kill cancer cells, and chemotherapy to treat cancer that has spread to other parts of the body.
How is melanoma skin cancer treated?
Melanoma skin cancer may require more aggressive treatment than non-melanoma skin cancers. Treatment options can include surgery, targeted therapy, immunotherapy, and sometimes radiation therapy, depending on the extent of the disease and the individual's overall health.
What are the complications of Skin Cancer treatment?
While treatment for skin cancer is generally effective, some individuals may experience complications such as infection at the surgical site, scarring or side effects from radiation or chemotherapy. These complications are typically managed by healthcare providers to ensure the best possible outcome for the patient.
Why is early diagnosis of skin cancer important?
Early diagnosis of skin cancer is crucial as it can significantly improve the prognosis and increase the likelihood of successful treatment. When cancer is detected at an early stage, it is often more manageable and may require less aggressive treatment.
What are the risks if skin cancer is not diagnosed early?
Delayed diagnosis of skin cancer can result in cancer cells spreading to other parts of the body, making treatment more challenging and decreasing the chances of a favourable outcome. Timely detection and intervention are key in preventing the progression of the disease.
How can individuals protect their skin to prevent skin cancer?
To reduce the risk of developing skin cancer, individuals should protect their skin from harmful UV rays by using sunscreen, wearing protective clothing, and seeking shade during peak sun hours. Regular self-examinations and skin checks by healthcare professionals are also essential for early detection.
When should you get your skin checked for skin cancer?
What is the recommended frequency of skin checks for early detection?
It is advisable to have regular skin checks, especially if you have a history of skin cancer, significant sun exposure, or a family history of the disease. Dermatologists recommend annual skin exams for most individuals to ensure early detection of any suspicious changes.
How can you perform self-examinations to check for skin cancer?
Self-examinations involve carefully inspecting your skin for any changes, including the development of new moles or spots, changes in existing moles or unusual skin growths. It is important to be vigilant and seek medical attention if you notice any worrisome signs.
What are the signs that indicate you should see a dermatologist for a skin check?
If you notice any new or changing spots on your skin, experience persistent itching or bleeding or have a family history of skin cancer, it is advisable to consult a dermatologist for a comprehensive skin check. Early detection can significantly improve treatment outcomes.
What is a skin biopsy and how is it used in skin cancer diagnosis?
What is the procedure for a skin biopsy?
A skin biopsy involves the removal of a small sample of skin tissue for examination under a microscope. The procedure is typically performed under local anesthesia and can help determine whether cancer cells are present, the type of skin cancer and the extent of the disease.
How are the results of a skin biopsy used in diagnosing skin cancer?
The results of a skin biopsy play a crucial role in diagnosing skin cancer, as they provide information about the presence of cancer cells, their characteristics and how advanced the disease may be. This information guides healthcare providers in developing an appropriate treatment plan.
What are the different types of skin biopsies, and when are they used?
Different types of skin biopsies include shave biopsy, punch biopsy and excisional biopsy, each used depending on the suspected nature of the skin condition. Shave biopsies are commonly performed for superficial lesions, while punch or excisional biopsies are used for deeper or larger lesions.
-
If I have a lot of moles, does my risk of melanoma increase?
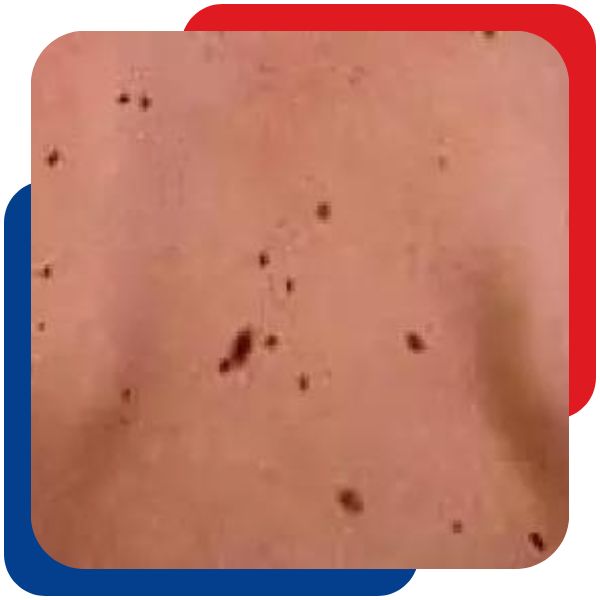
Large numbers of moles are associated with both a genetic predisposition to mole formation and increased sun exposure in childhood as a trigger for mole formation.
Moles in at-risk individuals, tend to cluster in areas of previous sun exposure and sun damage, including areas that have been sunburnt in the past. In this way, large numbers of moles can act as a marker for people at increased risk of both melanoma and non-melanoma skin cancer (such as BCC and SCC).
If you have large numbers of moles, particularly if you have odd-looking or asymmetric-appearing moles, then a regular (at least annual) skin check with an experienced skin cancer doctor is recommended because you may be at higher risk of melanoma, particularly with advancing age, although melanoma can occur in any age group.
Detect Early Signs of Cancerous Moles or Melanoma Skin Cancer
Many people may not realize that regular monitoring of moles on the skin is crucial for detecting early signs of melanoma, a type of skin cancer that can be life-threatening if not treated promptly. Understanding the features of melanoma and its relationship to moles is essential for early detection and effective treatment.
Understanding Melanoma
Melanoma is a type of skin cancer that develops in the cells that produce melanin, the pigment responsible for skin colour. It often starts in moles but can also occur in other pigmented tissues. One key aspect to note is that not all moles are cancerous; however, monitoring them for changes is important as melanoma can arise from existing moles or manifest as new ones.
What are the risk factors associated with melanoma skin cancer?
Several risk factors contribute to the development of melanoma, including exposure to ultraviolet (UV) radiation from the sun or tanning beds, having fair skin, a history of sunburns, and having many moles on the body. Individuals with a family history of melanoma are also at a higher risk of developing the disease.
How do common moles differ from atypical moles in terms of melanoma risk?
Common moles are usually harmless and are typically round or oval with a smooth border and a uniform colour. Atypical moles, also known as dysplastic nevi, are irregular in shape, size, and colour. While common moles have a low risk of developing melanoma, atypical moles are considered precancerous and increase the risk of melanoma.
Skin Cancer: Types and Risks
Aside from melanoma, there are other types of skin cancer such as basal cell carcinoma and squamous cell carcinoma. Melanoma is the most serious type and can rapidly spread to other parts of the body if not treated early. Factors like a family history of melanoma, a personal history of skin cancer, and exposure to UV radiation can increase the risk of developing melanoma.
What is the significance of family history in relation to melanoma risk?
A family history of melanoma increases the risk of developing the disease due to genetic predisposition. Individuals with close relatives who have had melanoma are at a higher risk themselves. Regular skin checks and early detection are crucial for those with a family history of melanoma.
Identifying Symptoms and Diagnosis
Recognizing the symptoms of melanoma is essential for early diagnosis and treatment. Common signs include changes in the size, shape, or colour of moles, or the appearance of new moles that exhibit irregularities. If any suspicious changes are noticed, seeking medical evaluation is necessary for proper diagnosis.
How is melanoma diagnosed and what are the key indicators?
Diagnosing melanoma typically involves a skin examination, dermoscopy, biopsy, and sometimes additional imaging tests. Key indicators of melanoma include asymmetry, irregular borders, varied colours, a large diameter, and evolving features of a mole. Personal and family history also play a role in the diagnosis.
Treatment and Screening
Treatment options for melanoma depend on the stage of the cancer and may include surgery, chemotherapy, radiation therapy, immunotherapy, or targeted therapy. Regular screenings are important for individuals at risk of melanoma to detect any changes in moles early and prevent the progression of the disease.
What considerations are there for people with a personal history of melanoma?
Individuals with a personal history of melanoma require close monitoring of their skin, as they have an increased risk of developing additional melanomas. They should adhere to regular skin self-exams and follow-up appointments with dermatologists to ensure timely detection and treatment of any new cancerous lesions.
Prevention Strategies and Risk Management
To reduce the risk of developing melanoma, avoiding excessive sun exposure, using sunscreen, wearing protective clothing, and seeking shade during peak sun hours are essential preventive measures. Understanding personal risk factors and practising sun safety can significantly reduce the likelihood of developing skin cancer.
What role does exposure to the sun play in the development of melanoma?
Exposure to UV radiation from the sun is a primary risk factor for melanoma. Prolonged or intense exposure can damage skin cells and increase the risk of developing cancerous lesions. Protecting the skin from harmful UV rays through sun-safe behaviours is crucial in preventing melanoma and other skin cancers.
Q: What are the risk factors for developing melanoma?
A: Risk factors for developing melanoma include having a family history of melanoma, having atypical moles, and being exposed to the sun for long periods.
Q: How is melanoma diagnosed?
A: Melanoma is diagnosed through a biopsy, where a small sample of the mole or suspicious skin lesion is removed and examined under a microscope.
Q: What are the symptoms of melanoma?
A: Symptoms of melanoma include changes in the size, shape, or colour of a mole, the development of new moles, or the presence of itching, bleeding, or pain in a mole.
Q: Is a family history of melanoma a significant risk factor?
A: Yes, having a family history of melanoma increases the risk of developing the disease due to genetic factors that may predispose individuals to skin cancer.
Q: What are the various types of skin cancer?
A: Melanoma is a type of skin cancer that originates in melanocytes, while non-melanoma skin cancers include basal cell carcinoma and squamous cell carcinoma.
Q: What treatments are available for melanoma?
A: Treatments for melanoma may involve surgery, chemotherapy, radiation therapy, immunotherapy, targeted therapy, or a combination of these depending on the stage and severity of the cancer.
Q: How important is early detection in the treatment of melanoma?
A: Early detection of melanoma is crucial as it increases the chances of successful treatment and improves the overall prognosis for individuals diagnosed with the disease.
MELANOMA SCAN - SKIN CANCER CLINIC
For further information, please feel free to Contact Us or follow the link to request an appointment by clicking Book Now.
-
Mole Removal
Not all moles are dangerous but sometimes the location can be annoying causing irritation. At Melanoma Scan we perform cosmetic mole removal with simple in-house surgical procedures.
-
New Skin Cancer Clinic in Warner

-
Photodynamic Therapy (PDT)

Photodynamic Therapy (PDT) is a unique way to treat thin cancers, sun damaged, blemished and aged skin on all areas of the body.
-
Signs of Skin Cancer

Skin cancer checks are an essential part of life for all people living in Queensland, a state with one of the highest rates of skin cancer in the world. Skin cancer check might involve monitoring changes in spots, new spots, persistent irritation, red or scaly marks, spots that bleed easily, and new lumps. You might notice a spot that's changing, growing, or simply looks different from the rest. Being vigilant about these changes always check your skin and promptly see your doctor or get a professional skin check if you notice any of these signs. Early detection is key to successful treatment, especially with signs of melanoma, which can be life-threatening if not diagnosed and treated promptly. Skin checks are recommended for all adults living in Australia, as part of normal care with your general practitioner
Who Has The Highest of Skin Cancer Risk?
An annual skin check (or more frequent checks) is recommended for adults if:
- you have a history of skin cancer or dysplastic naevus syndrome (abnormal mole)
- you have an extensive history of sun exposure.
- you have a family history of skin cancer or dysplastic naevus syndrome (abnormal moles)
- you have premalignant change on your skin (solar keratosis)
- you have a large number of moles on your skin
- your doctor has recommended a regular check.
What are Skin Cancer Warning Signs and Symptoms?
Skin cancers can be sometimes obvious but more often subtle changes in your skin. Any change in your skin can alert you to the risk of skin cancer but in particular it is important to watch out for:
- any change in a mole or pigmented spot on your skin
- any new pigmented spot on your skin, particularly if it changes after you first notice it.
- any persisting itch or irritation in a mole or other spot on your skin
- any persisting red scaly mark, particularly if it grows over time.
- any spot that bleeds easily, for instance, with towelling after bathing
- any new lump that arises, particularly if it grows after you first notice it.
If you have noticed any of these changes on your skin, you should present immediately to your general practitioner or skin cancer doctor for a check.
What are the Different types of Skin Cancer?
The three main types of skin cancer are basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma. BCC is the most common and grows slowly, while SCC can grow quickly. The causes of skin cancer are primarily linked to exposure to UV radiation, with risk factors including skin type, sun exposure, and a history of skin cancer. Australia has a high rate of skin cancer, and at Melanoma Scan, we encourage awareness, prevention, and early detection.
Basal Cell Carcinoma
Basal cell carcinoma (BCC) is the most prevalent type, constituting approximately 66% of skin cancers, and originates in the basal cells of the skin. Typically, BCC exhibits slow growth over several months or years and seldom metastasises to other body parts. If left untreated, certain BCCs can penetrate deeper into the skin, affecting nerves and adjacent tissues, posing challenges for treatment.
The likelihood of developing additional BCCs increases if one has already been diagnosed, and it's possible to have multiple BCCs simultaneously in different areas of the body.
Signs of BCC include:
- Occurs in regions with heightened sun exposure, such as the head, face, neck, shoulders, lower arms, and legs, though it can manifest anywhere on the body.
- Presents as a pearl-coloured lump or slightly scaly area that appears shiny and pale, bright pink, or potentially darker.
- May result in the breakdown of the skin (ulceration), bleeding, and inflammation. The affected area may seem to heal and then become inflamed once again.
Squamous Cell Carcinoma
Squamous cell carcinoma (SCC) constitutes the second most common type of skin cancer, accounting for about 33% of cases. Originating in the squamous cells of the skin, SCCs have the potential for rapid growth over several weeks or months.
Some SCCs are confined to the top layer of the skin, termed SCC in situ, intra-epidermal carcinoma, or Bowen’s disease. When SCC invades through the basement membrane, it is categorised as invasive SCC. If left untreated, invasive SCC can metastasise to other parts of the body. SCC occurring on the lips and ears is more prone to spreading.
Signs of SCC include:
- Typically appearing on areas of the body frequently exposed to the sun, such as the head, neck, hands, forearms, and lower legs, but can initiate anywhere.
- Often presenting as a thickened, red, scaly, or crusted spot or a rapidly growing lump.
- May exhibit bleeding, inflammation, and tenderness upon touch.
Melanoma
Melanoma, a form of skin cancer, originates in melanocytes and typically develops on areas of the body that have undergone excessive sun exposure. Uncommonly, melanomas may initiate within the eye or in regions of the skin or body unaffected by sunlight, including mucous membranes (e.g., sinuses, digestive tract, genitals), soles of the feet, palms of the hands, and beneath the nails. Despite being less prevalent than non-melanoma skin cancer, melanoma is deemed highly serious due to its increased likelihood of spreading to various body parts, particularly when not identified in its early stages.
Signs of Melanoma include:
Melanoma exhibits diverse appearances, especially in individuals with numerous moles, making it distinct from other moles. The initial indication often involves a new spot or alterations in an existing mole, characterised by:
Size:The spot may emerge or commence growing larger.
Colour: The spot may display irregular blotches with varying depths and hues, including brown, black, blue, red, white, light grey, pink, or skin-coloured.
Shape or Border:The spot may elevate, develop scaliness, adopt an irregular shape (scalloped or notched), or lack symmetry, presenting different halves.
Itching or Bleeding:The mole may be prone to easy itching or bleeding.
Elevation:The spot may initiate as a raised nodule or evolve into a raised area, often taking on a reddish or reddish-brown hue.What Can Happen if I Don't Get a Skin Check?
The most important factor in skin cancer care is the prompt recognition of a skin cancer and it's early and complete removal. Melanoma in particular can be deadly if there is a delay in diagnosis. The chance of a person dying from melanoma is most closely related to the thickness of the melanoma at the time of initial diagnosis and any evidence of early spread. In most cases, with prompt recognition and treatment, the chance of dying from melanoma is rare (level 1 melanoma has a 5-year survival rate of >99%), however, in some cases the melanoma has already spread from the initial site where it arose, and in this situation treatment options can be limited. The chance of an individual patient dying from a melanoma has dropped in the last 10 years due to early recognition and treatment of this cancer, so don't delay if you believe you may have one.
Regular Skin Checks is the best course of defence against Early Skin Cancer Detection
In the pursuit of a healthy life, your first line of defence against skin cancer is regular check-ups. Living in Queensland, where skin cancer rates are among the highest globally, it's crucial to be proactive in your healthcare. Whether you've noticed changes or not, an annual skin check, especially if you have a history of skin issues, sun exposure, or a family history, can make all the difference.
Don't underestimate the power of early detection – it can be a lifesaver. Reach out to our dedicated skin cancer clinics in Brisbane Northside or consult with your GP. Remember, your skin's well-being is in your hands, and the key to effective diagnosis and treatment lies in regular check-ups. Take charge of your health and schedule a skin check today.
-
Skin Cancer Surgery

Our skin cancer doctors are also skilled surgeons. This means that if a skin cancer is found, the Doctor can remove the lesion at the time of the initial consultation. A biopsy is always performed to identity the type of skin cancer and if further treatment options are required.
-
Skin Cancer Treatment
Skin Cancers can be Treated Using Surgical and Non-Surgical Treatments
Surgical treatments used for treatment of skin cancers are physical treatments to remove the tumour. Depending on the thickness of the lesion the treatment may be more or less invasive. Thicker tumours are generally treated with excision and techniques include elipse (boat shaped excision), flaps and grafts. On occasion the wound may be left open for a period of time to await results of histopathology (as in the so called 'Slow Moh's'), but in most cases the wound is closed immediately following the removal of the tumour. Surgical treatments also include diathermy and serial curettage. This is usually used for superficial tumours on areas of the body where recurrence is less likely. Both small and large tumours can be treated with this technique.
Non-surgical treatments are treatments using medications to attack and remove the tumour. They include Aldara (Imiquimod), Efudix, and Metvix PDT (Photodynamic therapy). These treatments are generally used for lesions which are thin and on areas of the body where recurrence is less likely, although small superficial lesions on higher-risk areas may be suitable for these treatments.
-
Wedge Excision
Wedge excision is a technique used to remove cancers from the edge of the lip, ear or eyelid.
-
What can I do to reduce scarring?
The Melanoma Scan doctor and nurse will give you detailed instructions on how to care for your wound to reduce scarring.
Shave excisions
With Shave excisions, the best results can be achieved using moist wound healing, using antibiotic ointments such as chloromycetin ointment or otocomb on high risk areas for infection, or using strataderm or stratamed silicone containing gels for areas at risk of keloid scarring. For some areas simple moist wound dressings using Vaseline, antiseptic creams or pawpaw ointment may be a low cost and suitable alternative. Your doctor will recommend the treatment that he believes is most suitable for your particular wound and situation.
Ellipse excisions
With ellipse excisions, taping is an important aspect of wound care to prevent a stretched up scar despite the support of the deep sutures. Equally important is abstaining where possible from exercise for up to 6 weeks following surgery. That may not always be possible with people engaged in manual work, but often with care and getting assistance with lifting and carrying, stretching of the scar can be minimised.
Keloid scarring is a feared outcome for all excisions, however is very uncommon outside of a small group of people who appear to be prone to them. In this group, silicone gels are utilised and the wound is reviewed 3-4 weeks after surgery to see if there is any sign of keloid formation, which can often appear after apparently normal early healing as a raised red itchy and uncomfortable scar. Occasionally steroid injections may be used to halt keloid formation or reduce an established keloid scar, but the results are not always satisfactory in this keloid prone group of patients.
Melanoma Scan - Skin Cancer Clinic
Minimising Scars After Surgery for Skin Cancer Treatment
Scars are a natural part of the healing process, especially after skin cancer surgery such as Mohs surgery. While the removal of cancerous cells is crucial, many individuals are concerned about the appearance of scars post-surgery. Fortunately, there are several effective methods and treatments available to minimise scarring and improve the overall appearance of the skin.
What Are Effective Ways to Reduce Scarring Post Skin Cancer Removal?
Minimising scarring with proper care is essential in promoting optimal wound healing and reducing the appearance of scars. Following post-operative care instructions, such as keeping the surgical site clean and avoiding excessive sun exposure, can aid in scar prevention. Using silicone gel for scar reduction is a popular method that helps flatten and fade scars over time, improving the skin's appearance.
Sunscreen plays a crucial role in scar prevention by protecting the skin from harmful UV rays that can darken scars and hinder the healing process. Regular application of sunscreen on the scarred area can help prevent discoloration and promote better scar healing, leading to improved overall skin health.
What Are the Treatment Options to Reduce the Appearance of Existing Scars?
Skin grafts are commonly used in scar revision to improve the appearance of existing scars. This procedure involves transferring healthy skin to the scarred area to promote better healing and reduce scar visibility. Utilising injections for scar tissue reduction is another effective method that can help break down scar tissue and improve the overall texture of the skin.
Benefits of silicone in scar management are well-documented, as silicone sheets or gels can help hydrate the scarred area and improve its elasticity, ultimately leading to a smoother and less noticeable scar. Incorporating silicone products into a scar care routine can significantly enhance the appearance of existing scars.
How Can Keloid Scars Be Prevented or Treated?
Understanding keloid formation and treatment is crucial in preventing and managing keloid scars. Keloids are raised scars that extend beyond the original incision site and can be challenging to treat. Effective methods to reduce the likelihood of keloid scarring include using pressure garments or silicone sheets to help flatten and soften the scars.
Various techniques, such as cryotherapy or laser therapy, can be utilised to minimise keloid scars by targeting excess scar tissue and promoting a more even skin texture. By implementing a comprehensive treatment plan that addresses the specific characteristics of keloid scars, individuals can effectively manage and improve the appearance of these challenging scar types.
For further information, please feel free to Contact Us or follow the link to request an appointment by clicking Book Now.


