Skin check
-
What causes skin cancer?
What causes skin cancer?
The vast majority of skin cancers are caused by exposure to ultraviolet light in the form of sun exposure but also from artificial sources such as solariums and arc welding. Other causes of skin cancer include exposure to cancer causing chemicals such as arsenic, or ionising radiation. These causes are much less common than ordinary sunburn from the sun. There are many types of skin cancers. Many Australians are burnt on a regular basis, and sunburns are often associated with outdoor activities we spend our leisure time doing, such as outdoor sports, gardening and swimming. Many outdoor workers are also burnt frequently although workplace health and safety preventionhas helped to some degree.
Understanding Skin Cancer: Risk Factors and Cancer Council
Skin cancer is a prevalent form of cancer that affects millions of people worldwide. Understanding the risk factors associated with this disease is crucial for prevention and early detection. The Cancer Council plays a vital role in raising awareness about skin cancer and promoting sun protection practices.
What is Skin Cancer?
Skin cancer is a type of cancer that originates in the skin cells. It can manifest in various forms, with the most common types being basal cell carcinoma, squamous cell carcinoma, and melanoma. These cancers often present with distinct signs that should not be ignored.
Definition of skin cancer
Skin cancer is characterised by the abnormal growth of skin cells, often triggered when you are exposed to uv radiation.
Different Types of skin cancer
The main types of skin cancer include basal cell carcinoma, squamous cell carcinoma, and melanoma, each with its own characteristics and treatment options.
Common signs of skin cancer
Signs of skin cancer may include changes in skin growth, the appearance of new moles, or unusual skin discoloration. It is essential to regularly check your skin for any abnormalities.
What Are the Risk Factors for Skin Cancer?
You can get skin cancer from prolonged exposure to UV rays. UV radiation is a significant risk factor for the development of skin cancer. Prolonged exposure to UV rays, whether from the sun or tanning beds, can increase the likelihood of developing the disease.
UV radiation and skin cancer
UV radiation emitted by the sun or artificial sources can damage the DNA in skin cells, leading to mutations that may promote the growth of cancerous cells.
Skin type and skin cancer risk
Individuals with fair skin are at a higher risk of developing skin cancer compared to those with darker skin tones. Light-skinned individuals have less natural protection against UV radiation.
Exposure to UV radiation and skin cancer risk
Prolonged exposure to UV radiation without adequate protection can significantly increase your risk of developing skin cancer. It is crucial to take measures to shield your skin from harmful UV rays.
How Does UV Exposure Contribute to the Development of Skin Cancer?
UV rays have a profound impact on skin cells, causing damage that can lead to the formation of cancerous growths. Understanding how UV exposure affects the skin is essential for implementing preventive measures.
Impact of UV rays on skin cells
UV rays penetrate the top layers of the skin, causing damage to the DNA of skin cells and potentially triggering mutations that give rise to skin cancer.
Types of skin cancer caused by UV exposure
Basal cell carcinoma and squamous cell carcinoma are often linked to chronic sun exposure, while melanoma is more commonly associated with intense, intermittent sun exposure that causes sunburns.
How sun exposure increases your risk of skin cancer
Cancer is the most common in people who are massively exposed to the sun. Repeated sun exposure without protection can lead to cumulative skin damage, increasing the risk of developing various forms of skin cancer over time.
Understanding Non-Melanoma Skin Cancer
Non-melanoma skin cancer, which includes basal cell carcinoma and squamous cell carcinoma, is the most common form of skin cancer. Being aware of its characteristics and risk factors is essential for prevention.
Information about non-melanoma skin cancer
Non-melanoma skin cancer typically develops in the top layer of the skin and is often associated with UV exposure and cumulative sun damage.
Risk factors associated with non-melanoma skin cancer
Individuals with fair skin, a history of sunburns, or prolonged sun exposure are at an increased risk of developing non-melanoma skin cancer compared to people with dark skin. Regular skin checks are crucial for early detection.
Sun protection and prevention of non-melanoma skin cancer
Practicing sun protection measures such as wearing sunscreen, protective clothing, and seeking shade can help reduce the risk of non-melanoma skin cancer. Early detection and treatment are key to managing the disease effectively.
Importance of Skin Cancer Prevention and Early Detection
Preventing skin cancer involves taking proactive steps to protect your skin from UV radiation and being vigilant about any changes that may indicate a potential issue. Early detection through regular skin checks can lead to better treatment outcomes.
Steps to protect your skin from UV radiation
Protecting your skin from UV radiation involves wearing sunscreen, seeking shade during peak sunlight hours, and wearing protective clothing such as hats and sunglasses.
Signs that may lead to skin cancer diagnosis
Changes in existing moles, new skin growths, or persistent sores that do not heal should be evaluated by a dermatologist to rule out skin cancer. Prompt medical attention is crucial for timely diagnosis and treatment.
Role of Cancer Council in Skin Cancer Awareness
The Cancer Council plays a pivotal role in raising awareness about skin cancer, promoting sun safety initiatives, and providing resources for skin cancer prevention and early detection. Their position statements and support services are valuable in the fight against this common cancer.
There are many types of skin cancers. Many Australians are burnt on a regular basis, and sunburns are often associated with outdoor activities we spend our leisure time doing, such as outdoor sports, gardening and swimming. Many outdoor workers are also burnt frequently although workplace health and safety prevention has helped to some degree.
-
Are skin cancers genetic?
Skin cancers do occur more commonly in some families, but rather than being genetic as such, it can be that these families all experienced more sunburns due to habitual exposure to the sun through sport or other outdoor activities. There are rare genetic mutations that can lead to a very high risk of skin cancer, including Gorlin’s syndrome, which can lead to a high risk of BCC formation. Melanoma appears to be genetic in a small proportion of patients, but there is no genetic testing available as yet to quantify your risk of melanoma. If you have a family history of skin cancer including melanoma, you may be at increased risk of skin cancer, and it may be worthwhile having annual skin checks, especially if you have risk factors for skin cancer yourself.
-
Are there stitches involved?
Are there stitches involved?
Sutures are used for closure of ellipse excisions, and these need to be removed at 7-14 days, depending on the site. Most are removed at day 7 but lower legs take longer to heal.
Do I need to come back to have the stitches removed?
Deep sutures dissolve by themselves over an extended period of time, however if they poke out through the skin at any stage in the healing process, they are usually removed to allow the wound to close completely.
Shave excisions do not need sutures and heal up like a graze wound with appropriate dressings and wound care.
Melanoma Scan - Skin Cancer Clinic
Understanding the Mole Removal Process
What is mole removal, and why is it done?
Mole removal is a procedure performed to eliminate unwanted or suspicious moles from the skin. It is usually done for medical reasons, such as assessing a mole for skin cancer risk or removing a bothersome or aesthetically unpleasing mole.
What are the different methods of mole removal?
There are various methods of mole removal, including excision, where the mole is cut out with a scalpel, and laser removal, which uses high-intensity light to vaporise the mole. Another method is shaving, which involves using a blade to "shave" off the mole from the surface of the skin.
What is the importance of biopsy after mole removal?
Biopsy post-mole removal is crucial to determine if the removed mole was cancerous or precancerous. It helps in providing information about the nature of the mole cells and guides further treatment if needed.
Scar Management After Mole Removal
How do you care for the wound and scar post-mole removal?
After mole removal, it is essential to keep the wound clean and covered with a sterile bandage. Proper wound care helps prevent infection and promotes effective healing, leading to minimal scarring.
When do the stitches from mole removal usually come out?
The timeline for stitches removal after mole removal varies from patient to patient. Typically, stitches are removed within 1 to 2 weeks, depending on the location of the mole and the healing progress.
What can affect the appearance of the scar after mole removal?
Factors such as the size and depth of the mole, the healing process, and individual skin characteristics can influence the scar appearance after mole removal. Proper wound care and scar management techniques can help in reducing scar visibility.
Healing Process and Mole Removal Aftercare
What is the typical healing time after mole removal?
The healing time after mole removal varies but usually takes 2–4 weeks for the wound to completely heal. During this period, proper aftercare practices are crucial for optimal healing.
What are the recommended ointments or bandages for aftercare?
Ointments like petroleum jelly and sterile bandages are commonly recommended for aftercare post-mole removal. They help in keeping the wound moist and protected, promoting faster healing.
How do we recognise signs of infection during the healing process?
Signs of infection post-mole removal include increased redness, swelling, warmth around the wound, and pus drainage. If any of these signs are observed, it is important to seek medical attention promptly.
Risks and Complications of Mole Removal
What are the potential risks associated with mole removal?
Potential risks of mole removal include infection, scarring, bleeding, allergic reactions to anesthesia, and rare complications such as nerve damage. These risks can be minimised by following proper pre and post-operative care instructions.
Is there a risk of skin cancer recurrence after mole removal?
While the risk of skin cancer recurrence after mole removal is low, regular skin examinations and monitoring for any new or changing moles are important for the early detection of potential skin cancer.
How do we monitor the area for any signs of melanoma post-mole removal?
Regularly inspecting the area where the mole was removed for any signs of melanoma, such as changes in color, shape, or size, is crucial. Any suspicious changes should be reported to a healthcare provider promptly.
Expectations Following Mole Removal Surgery
What can one expect in terms of scarring after mole removal?
The extent of scarring after mole removal varies depending on factors like wound care, scar management, and individual healing responses. Proper care can help in minimising the appearance of scars.
Does the location of the mole impact healing time?
The location of the mole can affect healing time, with areas of the body that experience more movement or friction taking longer to heal. Following care instructions and keeping the wound clean are essential for timely healing.
When should one seek medical attention post-mole removal?
If any unusual symptoms like excessive pain, bleeding, signs of infection, or concerning changes in the wound or surrounding skin are observed post-mole removal, prompt medical attention should be sought.
For further information, please feel free to Contact Us or follow the link to request an appointment by clicking Book Now.
-
Basal Cell Carcinoma

Basal Cell Carcinoma (BCC) is the most common form of skin cancer. It is derived from the basal or deepest layers of the epidermis (outer layer of skin).
-
Book a PDT Light Therapy Assessment
PDT Light therapy (Photodynamic Therapy) is fast becoming a popular and effective treatment for pre-cancerous lesions and fields as well as some early cancers.
This therapy also has the added advantage of improving the look and feel of the skin.
Schedule an Appointment
A pre-treatment appointment should be completed 2-3 weeks prior to the light therapy treatment date.
Complete the form below and we will get back to you with the soonest available appointment.
Please note that the Light Therapy is currently only available in our Mitchelton Skin Cancer Clinic and our Toombul Skin Cancer Clinic in Nundah
-
Contact Us
Call us on 1300 754 000 and you will be directed to your local clinic.
Our clinic locations are listed below.Melanoma Scan Toombul
9 Parkland Street Nundah, Queensland 4012 Ph: 07 3256 6766
Melanoma Scan Warner
Warner Plaza, Shop 2 1405 Old North Road, Warner 4500 Ph: 07 3106 1340
Melanoma Scan Mitchelton
Unit 1/23 Blackwood Street, Mitchelton 4053 Ph: 07 3855 8500
Send us a message
-
Ellipse Excision
Ellipse excision is the simplest and commonest form of surgical treatment and involves cutting out a boat shaped section of skin containing the cancer, and then using sutures to bring the edges together.
-
How do I protect my children against skin cancer?
Sun damage at a young age is potentially the most dangerous, because the skin is thin and delicate and may burn more easily. It is also the time when sunburn is most likely to result in freckling and mole formation, which are both markers for people at risk of future skin cancers. In fact, a mole count over forearms is an indication of future melanoma risk, with high mole counts being associated with increased lifetime risk of melanoma. Children need to be protected from sun damage and in particular sun burn with hats, sunglasses, protective clothing (shirts, rash vests), high potency sunscreens (50+ SPF recommended) and avoidance sun exposure in the hottest part of the day. Every sunburn contributes to an increased risk of skin cancer in future and there may be a very long (decades) delay before the skin cancer appears. Skin cancers occurring after a single sunburn has been documented, with a delay of 40 years between the sunburn and the eventual cancer formation. Regular sunscreen application for skin types susceptible to sun burn can prevent accidental sunburns, and lead to a reduced risk of future skin cancers.
Most children are at very low risk of skin cancers, so regular skin checks are not routinely recommended unless there are particular concerns. While skin cancers including melanoma are rare, they do occur, so if there is a mole or spot that is changing or growing at an accelerated rate, or looks odd or different to every other mole on the child’s body, then they should be checked to ensure it is not a cancer.
Protecting Your Children from Skin Cancer: Sun Protection Tips
Exposure to the sun's harmful UV rays can have detrimental effects on our skin, especially for children whose skin is more delicate and prone to damage. Ensuring proper sun protection for your children is crucial in preventing the risk of skin cancer later in life.
Sun Protection against UV
Why is sun protection important for children? Effective sun protection is essential as children have sensitive skin that is more susceptible to skin damage from UV exposure. Without adequate protection, there is an increased risk of developing skin cancer in the future.
What are the risks of not using sun protection? Not using sun protection exposes children's skin to harmful UV rays, leading to skin damage and an elevated risk of skin cancer development.
How can you effectively protect your child from the sun? Ensuring good sun protection involves a combination of measures such as applying sunscreen regularly, seeking shade, and wearing protective clothing to shield the skin from harmful UV rays.
Sunscreen and Skin Cancer
How does sunscreen help prevent skin cancer? Quality sunscreen forms a protective barrier on the skin, blocking harmful UV rays that can contribute to skin cancer development.
What type of sunscreen is best for children? When choosing sunscreen for children, opt for broad-spectrum formulas with a high UV protection factor to ensure optimal sun protection.
What SPF should you look for in sunscreen? Look for a minimum SPF of 30 or higher to effectively shield your child's skin from damaging UV rays that can lead to skin cancer.
Skin Cancer in Children
What are the signs of skin cancer in children? Watch for unusual moles, sores that don't heal, or changes in existing moles on your child's skin, as these could indicate a potential risk of skin cancer.
How common is skin cancer in children? While less common than in adults, skin cancer can still affect children, making regular skin checks essential for early detection and treatment.
What factors contribute to skin cancer in children? Factors such as UV exposure, type of skin, and sun protection practices play a role in the development of skin cancer in children.
Protective Clothing and Sun Safety for reduced sun exposure
How does protective clothing help in sun protection? Wearing sun protective clothing shields the skin from harmful UV rays, providing an extra layer of defence against skin damage and skin cancer.
What should children wear to stay safe in the sun? Opt for lightweight, long-sleeved shirts, wide-brimmed hats, and sunglasses to safeguard your child's skin and eyes from UV exposure.
Are there clothing materials that offer better sun protection? Look for fabrics with a tight weave and darker colours, as they offer superior sun protection compared to light-coloured, loosely woven garments.
Sun Protection Measures for Babies and Children
Aside from sunscreen, what other measures can protect children from the sun? Seeking shade during peak UV hours, staying hydrated, and wearing sun-protective clothing are all essential components of comprehensive sun protection measures.
How important are sunglasses in sun protection? Sunglasses not only shield the eyes from UV rays but also reduce the risk of eye damage and skin cancer around the delicate eye area.
Essential awareness of sun protection times
What are the best times to practice sun protection? It is crucial to practice sun protection all year round, especially during summer months and between 10 am and 4 pm when UV levels are at their highest.
Regular Skin Checks
Most children are at very low risk of skin cancers, so regular skin checks are not routinely recommended unless there are particular concerns. While skin cancers, including melanoma, are rare, they do occur, so if there is a mole or spot that is changing or growing at an accelerated rate or looks odd or different to every other mole on the child’s body, then they should be checked to ensure it is not cancer.
-
How do I reduce scaring from my recent skin cancer removal?
The Melanoma Scan doctor and nurse will give you detailed instructions on how to care for your wound to reduce scarring.
Any procedure to remove a skin cancer will cause a scar and some people will scar more than others depending on their tendency towards keloid scarring and their skin type. Scars tend to settle to a pale mark, either an oval area after curettage and cautery or as a line from excisional skin surgery. If there is a lot of background sun damage, this pale area can become more prominent and noticeable. Background sun damage can include solar keratosis, freckles, pigmentation, age spots and telangiectasias (dilated small vessels on the skin surface). All of these lesions can be treated, either as individual lesions or as part of a field treatment such as edit, PDT, lazer, IPL or skin peels.
-
How long does it take to have a cosmetic mole removal?
Mole removal occurs in two ways, either a shave excision, which is very quick, or a formal ellipse excision, which takes a little longer. Shave excision is a technique that involves putting a small amount of local anaesthetic under the mole and then using either a straight or curved blade, which is passed through the skin directly under the mole, resulting in the mole being removed with a narrow margin of normal tissue under and around it. Occasionally, if the mole is being removed for benign reasons (for example, it is raised and gets in the way of shaving and repeatedly traumatised) the doctor may remove the raised part of the mole and leave a small amount of mole tissue behind, in an effort to minimise any visible scar or depression left by the mole removal. This procedure normally takes between two minutes and 5 minutes to do, using a low-sting local anaesthetic, which has the dual advantages of hurting less and giving almost immediate numbing to superficial lesions like a mole. This type of mole removal can often be incorporated into a skin check or 15-minute procedure time.
Formal ellipse excision takes a little longer, because a larger area of skin needs to be numbed, and a formal excision setup needs to be done by the doctor or nurse. The mole needs to be removed as an ellipse of skin (a boat-shaped piece of skin removed) and the wound sutured, usually in two layers, closing both deep and superficial parts of the skin, minimising the risk of scar stretching and tram track marks being left behind from the sutures. A typical mole removal using this technique takes about fifteen minutes to perform when assisted by a nurse, or 25 minutes without the assistance of a nurse.
Having a mole is a common occurrence for many individuals, as these small coloured spots on the skin are usually harmless. However, in some cases, mole removal may be necessary for both health and cosmetic reasons.
What is a Mole and Why Does It Need Removal?
Understanding the Nature of Moles on the Skin
A mole, also known as a nevus, is a growth on the skin that can appear anywhere on the body. Most moles are harmless and are usually brown or black in colour. They are made up of cells called melanocytes, which give the mole its pigmentation.
When Should You Consider Removing a Mole?
While most moles are benign, some may need to be removed if they show signs of change in size, shape, or colour. If a mole becomes itchy, and painful, starts bleeding, or exhibits asymmetrical borders, it is important to have it checked by a dermatologist.
Possible Risks Associated with Untreated Moles
Untreated moles that exhibit abnormal characteristics could potentially develop into skin cancer, particularly melanoma. Timely removal of suspicious moles can help prevent the progression of skin cancer.
Process of Mole Removal and Treatment Options
Types of Mole Removal Procedures Available
There are different methods of removing moles, including excision, laser therapy, shave excision, and radiofrequency ablation. The chosen method depends on the size, shape, and location of the mole.
Comparison of Cosmetic Mole Removal Techniques
Cosmetic mole removal techniques aim to remove the mole with minimal scarring. Laser mole removal and shave excision are popular cosmetic procedures that offer precise removal of moles with reduced scarring.
Discussing Treatment Options with a Skin Doctor
It is essential to consult a dermatologist to discuss the best treatment option for mole removal based on the individual's skin type, the mole's characteristics, and the desired outcomes.
Healing Process and Scar Care After Mole Removal
Expected Healing Time After Mole Removal
The healing time after mole removal varies depending on the method used and the size of the mole. Generally, it takes a few weeks for the skin to heal completely.
Scar Formation and Scar Healing Remedies
After mole removal, a scab will form, which will eventually fall off, leaving behind a scar. To aid in scar healing, applying silicone-based gels, keeping the scar moisturized, and protecting it from the sun can help minimize scarring.
Tips for Minimizing Scarring After Mole Removal
To reduce scarring after mole removal, it is important to follow post-procedure care instructions provided by the dermatologist, avoid picking at the scab, and keep the area clean and protected from infection.
Skin Cancer Concerns and Moles: What You Need to Know
Link Between Skin Cancer and Moles
Skin cancer, particularly melanoma, can develop from abnormal moles. Regular skin checks and monitoring moles for any changes are crucial in the early detection and treatment of skin cancer.
Identifying Signs of Melanoma in Moles
Signs of melanoma in moles include asymmetry, irregular borders, uneven colour distribution, and changes in size. If a mole shows any of these signs, immediate medical attention is necessary.
Importance of Timely Treatment for Suspicious Moles
If a mole appears suspicious or displays concerning features, such as rapid growth or changes in appearance, it is essential to seek professional evaluation and prompt treatment to prevent potential skin cancer development.
Scheduling Your Mole Removal Appointment and Aftercare
How to Book an Appointment for Mole Removal
To schedule a mole removal appointment, individuals can contact a skin specialist or a skin cancer clinic to arrange a consultation and discuss the removal procedure.
Preparation Steps Before Mole Removal Procedure
Prior to the mole removal procedure, patients may need to follow specific pre-operative instructions, which may include avoiding certain medications and preparing the skin surrounding the mole.
Post-Procedure Care for Optimal Healing and Recovery
After mole removal, following post-procedure care instructions, such as keeping the area clean, applying recommended ointments, and attending follow-up appointments, is essential for optimal healing and scar care.
Q: What is skin mole removal?
A: Skin mole removal is a procedure to remove moles from the skin that may be concerning or unwanted. It can be done for both cosmetic reasons and to prevent skin cancer.
Q: What is the healing time after mole removal?
A: The healing time after mole removal can vary depending on the method used and the size of the mole. It usually takes a few weeks for the skin to completely heal.
Q: What are the risks of scarring after mole removal?
A: Scarring after mole removal is a common concern, especially if the mole is large or located in a prominent area. However, with proper care and follow-up, scarring can be minimized.
Q: Is cosmetic mole removal an option?
A: Yes, cosmetic mole removal is an option for those who wish to have moles removed for aesthetic reasons. It can help improve the appearance of the skin and boost self-confidence.
Q: How can I book an appointment for mole removal?
A: You can book an appointment for mole removal by contacting a skin doctor or specialist skin clinic that offers mole removal services. They will assess your mole and recommend the best course of action.
Q: What is the process for scar healing after mole removal?
A: Healing after mole removal involves keeping the area clean and protected, following any post-procedure care instructions provided by your doctor, and monitoring the site for any signs of infection or complications.
Q: What are the different methods of mole removal?
A: The different methods of mole removal include surgical excision, laser removal, and cryotherapy. The method used will depend on the size and location of the mole, as well as other factors.
IS IT A STANDARD PROCEDURE TIME?
A shave excision can be done in a standard 15-minute appointment, however, an ellipse excision is usually booked into a 30-minute procedure appointment, so it depends on the technique that you have discussed with your doctor.
MELANOMA SCAN - SKIN CANCER CLINIC
For further information, please feel free to Contact Us or follow the link to request an appointment by Book Now.
-
How long will it take to heal?
The healing time is different for the two different types of mole removal and the location, and also the reason for the excision. The healing time of a cosmetic mole removal on a face can be 7-10 days, during which there will be a scab form and then fall off as the skin heals up under the scab. A deep shave excision for testing for possible melanoma is a much deeper and wider shave excision and depending on the location on the body, can take between 2 and 4 weeks to heal. There can be a risk of infection on the lower leg with this technique (or any excision on the lower leg) due to poor immune function and blood supply on the lower leg, which can further delay healing.
Ellipse excision on the face takes 7 days to heal enough for sutures to be removed, and other parts of the body usually take between 7 and 14 days to heal to the point where sutures can be removed. However, this is only the early stage of healing, with deep sutures continuing to support the wound for the next 6 weeks until further strength has developed in the wound. During this time, sporting activities, lifting, carrying, bending and squatting need to be avoided depending on the location of the wound, and the wound needs to be supported with taping with micropore tape or similar. Wound can be as little as at 10% of their eventual strength at day 7 without supportive deep sutures, and can reach 80% of their eventual strength at 3 months, hence the need to continue taping for an extended period and limit physical exertion, especially on the area affected by the surgery.
Melanoma Scan - Skin Cancer Clinic
Understanding that skin cancer is a type of cancer that originates in the skin cells is crucial. Skin cancer is the abnormal growth of skin cells, often as a result of damage caused by exposure to ultraviolet (UV) rays from the sun or tanning beds.
There are several types of skin cancer, including basal cell carcinoma, squamous cell carcinoma, and melanoma, each with varying risks and characteristics. Basal cell carcinoma is the most common and least dangerous, while melanoma is the most aggressive form of skin cancer.
The risks and complications associated with skin cancer can range from mild to severe, depending on the type and stage of the cancer. Early detection and effective treatment are essential in managing these risks and reducing the chances of complications.
Wound Care After Skin Cancer Excision
Following skin cancer excision, it is vital to adhere to specific care instructions to promote proper healing and prevent infections. Your healthcare provider will provide detailed post-procedure care guidelines tailored to your individual case.
Wound care plays a crucial role in the recovery process after skin cancer excision. Proper wound care tips include keeping the wound clean and dry, changing bandages regularly, and applying recommended ointments such as petroleum jelly to aid in healing.
Knowing when to seek help is essential during the recovery phase. If you experience excessive pain, swelling, redness, or drainage from the wound site, contact your healthcare provider immediately for guidance and assistance.
Scar Management and Suture Removal
Scar prevention and treatment are key aspects of managing the aftermath of skin cancer excision. Techniques such as massaging the scar tissue, applying silicone sheets, and using sunscreen to protect the area from UV exposure can help minimise scarring.
In some cases, skin grafts or flaps may be necessary to repair significant defects following skin cancer surgery. These procedures involve moving healthy skin from one area of the body to the site of excision to promote optimal healing and cosmetic outcomes.
The suture removal process is typically carried out by a healthcare professional to ensure proper wound closure. Following the removal of sutures, continued wound care is essential to support the healing process.
Aftercare for Different Types of Skin Cancer
After skin cancer excision, the aftercare process may vary depending on the type of skin cancer that was removed. For basal cell carcinoma, routine follow-up appointments with your skin cancer doctor is necessary to monitor for recurrence and address any concerns.
For squamous cell carcinoma, post-care instructions may involve regular skin checks, sun protection practices, and monitoring any changes in the surrounding skin. Early detection of any abnormalities is critical in preventing the spread of cancer.
After the excision of melanoma, close monitoring for any signs of recurrence or metastasis is essential. This may involve additional imaging studies, blood tests, and ongoing discussions with your medical team to ensure comprehensive aftercare.
For further information, please feel free to Contact Us or follow the link to request an appointment by clicking Book Now.
-
If I have a lot of moles, does my risk of melanoma increase?
Large numbers of moles are associated with both a genetic predisposition to mole formation and increased sun exposure in childhood as a trigger for mole formation.
Moles in at-risk individuals, tend to cluster in areas of previous sun exposure and sun damage, including areas that have been sunburnt in the past. In this way, large numbers of moles can act as a marker for people at increased risk of both melanoma and non-melanoma skin cancer (such as BCC and SCC).
If you have large numbers of moles, particularly if you have odd-looking or asymmetric-appearing moles, then a regular (at least annual) skin check with an experienced skin cancer doctor is recommended because you may be at higher risk of melanoma, particularly with advancing age, although melanoma can occur in any age group.
Detect Early Signs of Cancerous Moles or Melanoma Skin Cancer
Many people may not realize that regular monitoring of moles on the skin is crucial for detecting early signs of melanoma, a type of skin cancer that can be life-threatening if not treated promptly. Understanding the features of melanoma and its relationship to moles is essential for early detection and effective treatment.
Understanding Melanoma
Melanoma is a type of skin cancer that develops in the cells that produce melanin, the pigment responsible for skin colour. It often starts in moles but can also occur in other pigmented tissues. One key aspect to note is that not all moles are cancerous; however, monitoring them for changes is important as melanoma can arise from existing moles or manifest as new ones.
What are the risk factors associated with melanoma skin cancer?
Several risk factors contribute to the development of melanoma, including exposure to ultraviolet (UV) radiation from the sun or tanning beds, having fair skin, a history of sunburns, and having many moles on the body. Individuals with a family history of melanoma are also at a higher risk of developing the disease.
How do common moles differ from atypical moles in terms of melanoma risk?
Common moles are usually harmless and are typically round or oval with a smooth border and a uniform colour. Atypical moles, also known as dysplastic nevi, are irregular in shape, size, and colour. While common moles have a low risk of developing melanoma, atypical moles are considered precancerous and increase the risk of melanoma.
Skin Cancer: Types and Risks
Aside from melanoma, there are other types of skin cancer such as basal cell carcinoma and squamous cell carcinoma. Melanoma is the most serious type and can rapidly spread to other parts of the body if not treated early. Factors like a family history of melanoma, a personal history of skin cancer, and exposure to UV radiation can increase the risk of developing melanoma.
What is the significance of family history in relation to melanoma risk?
A family history of melanoma increases the risk of developing the disease due to genetic predisposition. Individuals with close relatives who have had melanoma are at a higher risk themselves. Regular skin checks and early detection are crucial for those with a family history of melanoma.
Identifying Symptoms and Diagnosis
Recognizing the symptoms of melanoma is essential for early diagnosis and treatment. Common signs include changes in the size, shape, or colour of moles, or the appearance of new moles that exhibit irregularities. If any suspicious changes are noticed, seeking medical evaluation is necessary for proper diagnosis.
How is melanoma diagnosed and what are the key indicators?
Diagnosing melanoma typically involves a skin examination, dermoscopy, biopsy, and sometimes additional imaging tests. Key indicators of melanoma include asymmetry, irregular borders, varied colours, a large diameter, and evolving features of a mole. Personal and family history also play a role in the diagnosis.
Treatment and Screening
Treatment options for melanoma depend on the stage of the cancer and may include surgery, chemotherapy, radiation therapy, immunotherapy, or targeted therapy. Regular screenings are important for individuals at risk of melanoma to detect any changes in moles early and prevent the progression of the disease.
What considerations are there for people with a personal history of melanoma?
Individuals with a personal history of melanoma require close monitoring of their skin, as they have an increased risk of developing additional melanomas. They should adhere to regular skin self-exams and follow-up appointments with dermatologists to ensure timely detection and treatment of any new cancerous lesions.
Prevention Strategies and Risk Management
To reduce the risk of developing melanoma, avoiding excessive sun exposure, using sunscreen, wearing protective clothing, and seeking shade during peak sun hours are essential preventive measures. Understanding personal risk factors and practising sun safety can significantly reduce the likelihood of developing skin cancer.
What role does exposure to the sun play in the development of melanoma?
Exposure to UV radiation from the sun is a primary risk factor for melanoma. Prolonged or intense exposure can damage skin cells and increase the risk of developing cancerous lesions. Protecting the skin from harmful UV rays through sun-safe behaviours is crucial in preventing melanoma and other skin cancers.
Q: What are the risk factors for developing melanoma?
A: Risk factors for developing melanoma include having a family history of melanoma, having atypical moles, and being exposed to the sun for long periods.
Q: How is melanoma diagnosed?
A: Melanoma is diagnosed through a biopsy, where a small sample of the mole or suspicious skin lesion is removed and examined under a microscope.
Q: What are the symptoms of melanoma?
A: Symptoms of melanoma include changes in the size, shape, or colour of a mole, the development of new moles, or the presence of itching, bleeding, or pain in a mole.
Q: Is a family history of melanoma a significant risk factor?
A: Yes, having a family history of melanoma increases the risk of developing the disease due to genetic factors that may predispose individuals to skin cancer.
Q: What are the various types of skin cancer?
A: Melanoma is a type of skin cancer that originates in melanocytes, while non-melanoma skin cancers include basal cell carcinoma and squamous cell carcinoma.
Q: What treatments are available for melanoma?
A: Treatments for melanoma may involve surgery, chemotherapy, radiation therapy, immunotherapy, targeted therapy, or a combination of these depending on the stage and severity of the cancer.
Q: How important is early detection in the treatment of melanoma?
A: Early detection of melanoma is crucial as it increases the chances of successful treatment and improves the overall prognosis for individuals diagnosed with the disease.
MELANOMA SCAN - SKIN CANCER CLINIC
For further information, please feel free to Contact Us or follow the link to request an appointment by clicking Book Now.
-
Keratoacanthoma
Some experts in skin cancer regard Keratoacanthoma (KA) as a subtype of SCC, but with the difference that they may eventually resolve without treatment if left alone.
-
Maintaining Healthy Skin: Sun Safety Tips and Best Practices

Maintaining healthy skin goes beyond just using skincare products. It also involves adopting sun safety practices to protect your skin from the damaging effects of the sun's harmful rays.
-
Mole Removal
Not all moles are dangerous but sometimes the location can be annoying causing irritation. At Melanoma Scan we perform cosmetic mole removal with simple in-house surgical procedures.
-
Photodynamic Therapy (PDT)

Photodynamic Therapy (PDT) is a unique way to treat thin cancers, sun damaged, blemished and aged skin on all areas of the body.
-
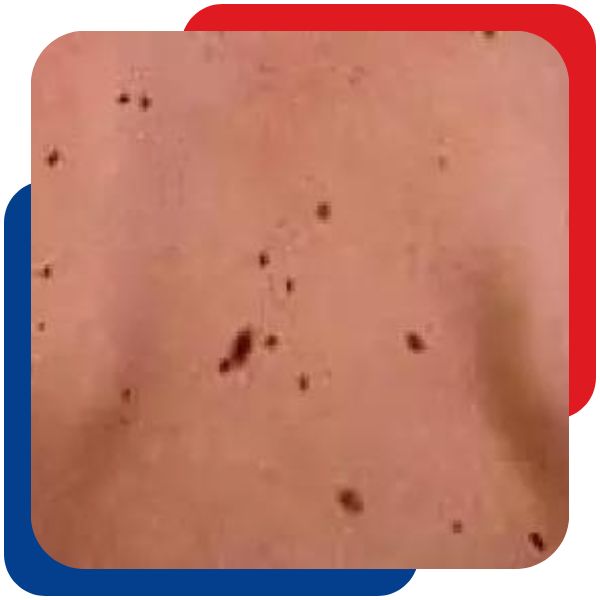
Signs of Skin Cancer

Skin cancer checks are an essential part of life for all people living in Queensland, a state with one of the highest rates of skin cancer in the world. Skin cancer check might involve monitoring changes in spots, new spots, persistent irritation, red or scaly marks, spots that bleed easily, and new lumps. You might notice a spot that's changing, growing, or simply looks different from the rest. Being vigilant about these changes always check your skin and promptly see your doctor or get a professional skin check if you notice any of these signs. Early detection is key to successful treatment, especially with signs of melanoma, which can be life-threatening if not diagnosed and treated promptly. Skin checks are recommended for all adults living in Australia, as part of normal care with your general practitioner
Who Has The Highest of Skin Cancer Risk?
An annual skin check (or more frequent checks) is recommended for adults if:
- you have a history of skin cancer or dysplastic naevus syndrome (abnormal mole)
- you have an extensive history of sun exposure.
- you have a family history of skin cancer or dysplastic naevus syndrome (abnormal moles)
- you have premalignant change on your skin (solar keratosis)
- you have a large number of moles on your skin
- your doctor has recommended a regular check.
What are Skin Cancer Warning Signs and Symptoms?
Skin cancers can be sometimes obvious but more often subtle changes in your skin. Any change in your skin can alert you to the risk of skin cancer but in particular it is important to watch out for:
- any change in a mole or pigmented spot on your skin
- any new pigmented spot on your skin, particularly if it changes after you first notice it.
- any persisting itch or irritation in a mole or other spot on your skin
- any persisting red scaly mark, particularly if it grows over time.
- any spot that bleeds easily, for instance, with towelling after bathing
- any new lump that arises, particularly if it grows after you first notice it.
If you have noticed any of these changes on your skin, you should present immediately to your general practitioner or skin cancer doctor for a check.
What are the Different types of Skin Cancer?
The three main types of skin cancer are basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma. BCC is the most common and grows slowly, while SCC can grow quickly. The causes of skin cancer are primarily linked to exposure to UV radiation, with risk factors including skin type, sun exposure, and a history of skin cancer. Australia has a high rate of skin cancer, and at Melanoma Scan, we encourage awareness, prevention, and early detection.
Basal Cell Carcinoma
Basal cell carcinoma (BCC) is the most prevalent type, constituting approximately 66% of skin cancers, and originates in the basal cells of the skin. Typically, BCC exhibits slow growth over several months or years and seldom metastasises to other body parts. If left untreated, certain BCCs can penetrate deeper into the skin, affecting nerves and adjacent tissues, posing challenges for treatment.
The likelihood of developing additional BCCs increases if one has already been diagnosed, and it's possible to have multiple BCCs simultaneously in different areas of the body.
Signs of BCC include:
- Occurs in regions with heightened sun exposure, such as the head, face, neck, shoulders, lower arms, and legs, though it can manifest anywhere on the body.
- Presents as a pearl-coloured lump or slightly scaly area that appears shiny and pale, bright pink, or potentially darker.
- May result in the breakdown of the skin (ulceration), bleeding, and inflammation. The affected area may seem to heal and then become inflamed once again.
Squamous Cell Carcinoma
Squamous cell carcinoma (SCC) constitutes the second most common type of skin cancer, accounting for about 33% of cases. Originating in the squamous cells of the skin, SCCs have the potential for rapid growth over several weeks or months.
Some SCCs are confined to the top layer of the skin, termed SCC in situ, intra-epidermal carcinoma, or Bowen’s disease. When SCC invades through the basement membrane, it is categorised as invasive SCC. If left untreated, invasive SCC can metastasise to other parts of the body. SCC occurring on the lips and ears is more prone to spreading.
Signs of SCC include:
- Typically appearing on areas of the body frequently exposed to the sun, such as the head, neck, hands, forearms, and lower legs, but can initiate anywhere.
- Often presenting as a thickened, red, scaly, or crusted spot or a rapidly growing lump.
- May exhibit bleeding, inflammation, and tenderness upon touch.
Melanoma
Melanoma, a form of skin cancer, originates in melanocytes and typically develops on areas of the body that have undergone excessive sun exposure. Uncommonly, melanomas may initiate within the eye or in regions of the skin or body unaffected by sunlight, including mucous membranes (e.g., sinuses, digestive tract, genitals), soles of the feet, palms of the hands, and beneath the nails. Despite being less prevalent than non-melanoma skin cancer, melanoma is deemed highly serious due to its increased likelihood of spreading to various body parts, particularly when not identified in its early stages.
Signs of Melanoma include:
Melanoma exhibits diverse appearances, especially in individuals with numerous moles, making it distinct from other moles. The initial indication often involves a new spot or alterations in an existing mole, characterised by:
Size:The spot may emerge or commence growing larger.
Colour: The spot may display irregular blotches with varying depths and hues, including brown, black, blue, red, white, light grey, pink, or skin-coloured.
Shape or Border:The spot may elevate, develop scaliness, adopt an irregular shape (scalloped or notched), or lack symmetry, presenting different halves.
Itching or Bleeding:The mole may be prone to easy itching or bleeding.
Elevation:The spot may initiate as a raised nodule or evolve into a raised area, often taking on a reddish or reddish-brown hue.What Can Happen if I Don't Get a Skin Check?
The most important factor in skin cancer care is the prompt recognition of a skin cancer and it's early and complete removal. Melanoma in particular can be deadly if there is a delay in diagnosis. The chance of a person dying from melanoma is most closely related to the thickness of the melanoma at the time of initial diagnosis and any evidence of early spread. In most cases, with prompt recognition and treatment, the chance of dying from melanoma is rare (level 1 melanoma has a 5-year survival rate of >99%), however, in some cases the melanoma has already spread from the initial site where it arose, and in this situation treatment options can be limited. The chance of an individual patient dying from a melanoma has dropped in the last 10 years due to early recognition and treatment of this cancer, so don't delay if you believe you may have one.
Regular Skin Checks is the best course of defence against Early Skin Cancer Detection
In the pursuit of a healthy life, your first line of defence against skin cancer is regular check-ups. Living in Queensland, where skin cancer rates are among the highest globally, it's crucial to be proactive in your healthcare. Whether you've noticed changes or not, an annual skin check, especially if you have a history of skin issues, sun exposure, or a family history, can make all the difference.
Don't underestimate the power of early detection – it can be a lifesaver. Reach out to our dedicated skin cancer clinics in Brisbane Northside or consult with your GP. Remember, your skin's well-being is in your hands, and the key to effective diagnosis and treatment lies in regular check-ups. Take charge of your health and schedule a skin check today.
-
Skin Cancer Check

Living in Australia you have a higher risk of skin damage as a result of increased exposure to the sun. Australians have a 2 in 3 chance of developing skin cancer in their lifetime. A simple yearly skin check can detect issues early and can save your life. Melanoma affects about 1 in 30 people in Australia and kills more than a 1000 people a year.
-
Skin Cancer Clinic Locations
Our three skin cancer clinics are located across the Northside of Brisbane.
-
Skin Cancer FAQ
Some Skin Cancer Frequently Asked Questions
What is skin cancer?
Skin cancer is a group of skin cells that have been damaged in a way that results in uncontrolled growth. Depending on the type of skin cancer, this can result in spread to distant sites in the body or locally destructive growth. Either forms of spread can result in damage to the body and eventual death if not treated.

What causes skin cancer?
The vast majority of skin cancers are caused by exposure to ultraviolet light in the form of sun exposure but also from artificial sources such as solariums and arc welding. Other causes of skin cancer include exposure to cancer causing chemicals such as arsenic, or ionising radiation. These causes are much less common than ordinary sunburn from the sun. Many Australians are burnt on a regular basis, and sunburns are often associated with outdoor activities we spend our leisure time doing, such as outdoor sports, gardening and swimming. Many outdoor workers are also burnt frequently although workplace health and safety prevention has helped to some degree.

What is sun burn and how can I prevent it?
Sunburn is the reaction of your skin to exposure to ultraviolet radiation from the sun. Depending on your skin type and the season, sunburn can occur after as little as ten minutes of sun exposure if adequate protection is not provided. Fair skin types and people with light coloured hair and eyes are the most prone to sun burn and hence to the subsequent development of skin cancer. Most Australians are aware of the danger of sun exposure, but sun burn is still very common because people underestimate the amount of ultraviolet radiation they are exposing themselves to. This includes days when it is overcast, cooler or windy, when the burning effects of the sun may not be noticed before a sunburn has already happened. All sunburns cause damage to the cells of your skin, and these changes include damage to the DNA of your cells. Over many years, enough damage to the DNA of your cells can accumulate to cause a skin cancer to develop. Many older people experience skin cancers many years after the activities that caused them have stopped, and may continue to have skin cancers appear from time to time despite minimal sun exposure.
Prevention of sun burn is through covering your skin with clothing, hats and sunglasses or through the use of sunscreens at all times when ultraviolet light is intense enough to damage your skin. This is typically between 10am and 3pm although this varies with season and climate. Here in Queensland in the summer months the UV index may be extreme from early morning though to early evening

Page 1 of 2


